The Recovery Time for a Lumbar Disc Herniation

Do you struggle with low back pain?
If so, the following story may sound all too familiar.
Recently, I had a patient, Matt, come into my office — hunched over in pain from spending the weekend bent over in his garden.
Whether you’re cleaning the yard or working in the garden, these tasks usually involve a lot of bending and lifting. Like many of us, Matt sacrificed lifting mechanics for time and ease.
These repetitive movements are not too kind to our spine and place a great deal of pressure on our discs. Unfortunately, Matt’s long hours of yard work turned into a lumbar disc herniation.
In a panic, Matt had a lot of questions: What caused this? What is the next step? When will the pain go away?
In order to answer these questions, we need a quick anatomy lesson first.
Lumbar Disc Herniation: Review of Anatomy
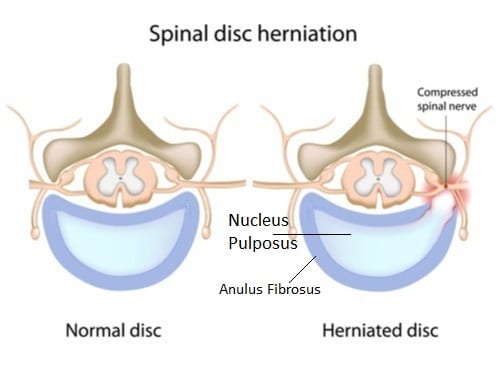
The discs in our back act as shock absorbers and cushioning between each vertebra of the spine. Think of these discs like jelly donuts. There is a fibrous outer shell called the annulus fibrous (the dough) and a gel (jelly) filled center called the nucleus pulposus.
When we bend, lift, or sit, there is a lot of pressure on the front side of the disc. This pressure can cause the back of the disc to push out.
A bulging disc occurs when the gel fluid breaks and moves into the outer shell, causing it to swell or deform.
A disc herniation occurs when the fluid breaks all the way through the outer shell and leaks into the spinal canal.
If the fluid or surrounding swelling from injury contacts one or more nerves exiting the spinal canal, you can present with pain, numbness, tingling, or weakness in the leg.
How Do We Stop the Fluid from Leaking?
To stop the pain, we need to stop the fluid from leaking. In order to heal, we must promote the optimal healing environment.
When we break a bone, the optimal healing environment is placing it in a cast. For your back, it isn’t quite that simple. You want to avoid positions that put pressure on the front of the disc. At the same time, you have to use postures that will help move the fluid or disc back to where it belongs.
Discs tend to do well with standing, walking, and exercises recommended by your Physical Therapist. These positions will place the load on the back of your disc and start to push the fluid inward.
Activities that will cause more fluid to leak are bending, lifting, twisting, sitting, and any impact (running or jumping). The more we stick to the “good” positions and limit the “bad,” the sooner our discs start to heal.
Tissue Healing Time
When your disc starts to leak fluid, it breaks through two barriers — an inner and outer layer of cartilage. Each layer of cartilage has its own healing timeline.
Typically, it takes three to four weeks for the fluid to stop leaking from the outer layer. Keep in mind, this only applies if you start limiting the bad positions and promoting those good positions.
At this time, the point of leakage will scar over and trap the fluid within the outer layer. This is the point in treatment when you can start to tolerate sitting for a little longer.
Over the next four weeks, the fluid will continue to work its way back toward the center of the disc, and eventually, the inner layer will scar over. This scarring traps the fluid back within the nucleus of the disc around the eight to twelve-week mark. Activities, such as bending forward and lifting (with the proper form of course), should be relatively pain-free.
When following the ideal plan, after about twelve weeks your disc is healed enough to tolerate impact, such as running or jumping.
Matt was not too pleased to hear that it will likely take at least three months to return to normal.
The best way to avoid having this discussion with a Physical Therapist is to prevent a disc injury from occurring in the first place.
Suffering a back injury may seem catastrophic, however, it does not mean you will have back issues for the rest of your life. With proper guidance, patience, and a little bit of hard work, you can heal your disc injury within twelve weeks!
Need help with your back pain?
If you’re struggling with a lumbar disc herniation or low back pain and would like a personalized plan to feel and move your best, our Physical and Occupational Therapists can help.
Treatment is covered by insurance, no referral is needed to start, and with flexible in-clinic and virtual appointments, you can find a time that fits your schedule.
Call 716-458-1990 or click below to get started:
